|
|
These tests should be performed during the first three days of the cycle,
preferably on an empty stomach. Some tests can be done on the 21st day
of the period. If the woman has no period, then the test can be performed
anytime
|
| |
| |

|
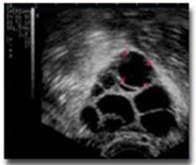
Ultrasound is a process whereby high-frequency sound waves, not radiation, are
transmitted through tissue. A thin ultrasound probe is inserted into the vagina
and the images on the screen are examined to evaluate the uterus and
ovaries.
A transvaginal ultrasound (TV USG) is the preferred route
for gynaecological evaluation as it gives more accurate information. Another
advantage is that it does not require a full bladder which can be very
uncomfortable for the patient. In fact, the bladder has to be emptied prior to
the scan. A thin ultrasound probe is inserted into the vagina and the images on
the screen are examined to evaluate the uterus and ovaries. The Fallopian tubes
cannot be evaluated by USG. Early
Endometriosis and adhesions may not be picked up on USG.
|
|
 |
| |
| |
|
TV USG is started on day 1,2 or 3 and then from day 9 onwards, every alternate
day, until ovulation. As the ultrasound waves strike the tissues, they project
a white image on the ultrasound screen. Follicles are round sacs of fluid
within the ovaries. Therefore, the follicles appear as dark circles on the
ultrasound screen. Each follicle contains an egg; however, the eggs cannot be
seen during the ultrasound. Ovulation, if occurring, would take place usually
by day 14 – 18. On an average, 5-6 visits are required to complete an
evaluation.
|
 |
|
 |
| |
| |
|
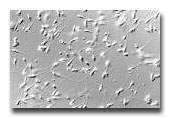
This is done 10-12 hrs after intercourse, around ovulation time, to check
whether the sperm is able to swim through the mucus at the mouth of the uterus
into the uterus to fertilise the egg. It is not a painful procedure. A speculum
is inserted into the vagina and the mucus sucked out very gently with a syringe
and placed on a slide. The slide is then examined under the microscope to look
for sperm and the test is graded.
|
 |
| |
| |
|
It is performed preferably after 2-3 days of abstinence. The semen should be
collected in a clean, sterilised bottle, provided by the laboratory. It should
be brought to the laboratory within ˝ hr of ejaculation, at room
temperature. Do not use ice while transporting the semen sample or collect
the semen in a condom and then transfer into the bottle for
examination. Do not use any lubricants locally.
|
 |
|
 |
| |
|
|
|
This is a short minor procedure ( approx. 15 mins), wherein radio
opaque dye is injected into the uterus,( via the vagina, through the mouth of
the uterus) and an X-Ray is taken to visualise the uterus and tubes. This
gives indirect information on the patency of the tubes and the shape of the
uterine cavity. It does not give information on the external surface of the
uterus, tubes and ovaries or of the pelvis behind these organs. It is usually
well tolerated and does not require anaesthesia and hence there is no need to
come fasting. Antibiotics are given routinely after the procedure and the
patient goes home immediately.
|
 |
| |
| |
|
This is a minimally invasive surgery and is also known as Band-aid
surgery. It is a day care surgical procedure. While the patient is under
general anesthesia, ( on an empty stomach) a one-half-inch incision is made in
the skin below the navel (umbilicus). Carbon dioxide is pumped into the abdomen
to make the organs of the pelvic cavity more easily visible.
The laparoscope, a narrow instrument similar to a telescope attached to a
fiberoptic flexible light cable, is inserted, allowing visual inspection of the
pelvic organs through a very tiny incision. This allows us to look for
abnormalities that lead to infertility without the need for major surgery. Many
conditions can be treated surgically too through additional small incisions in
the lower abdomen. The carbon dioxide gas is then released and the incisions
are stitched. There will be 1-2 stitches for a diagnostic laparoscopy and 3-4
stitches totally at the points of entry of the instruments for an
operative laparoscopic surgery. Patients are usually able to go home
within 4-6 hours of surgery.
Postoperative pain may be experienced (usually in the form of shoulder
pain) as a little carbon dioxide may remain and until it is absorbed, will
irritate the diaphragm( muscle separating the chest from the abdomen). Since
the diaphragm has the same nerve supply as the shoulder, the ‘referred pain’
will be experienced there.
|
|
Often a hysteroscopy is performed at the same time as a laparoscopy especially
in women who are undergoing an infertility investigation.
|
 |
| |
| |
|
This is another form of a minimally invasive surgery. It is an outpatient
procedure , performed under general anaesthesia. An Hysteroscope, a narrow
fiberoptic telescope is inserted into the uterus through the mouth of the
uterus to look inside. Therefore, it is not necessary to make an incision.
Either fluid or gas is used to distend the uterine cavity during hysteroscopy.
The uterine cavity is then inspected for any abnormality on a video monitor.
The shape of the uterus and the lining of the uterus are examined. Any evidence
of intrauterine pathology is looked for. The openings to the fallopian tubes
(tubal ostia) are also visualised.
Several different instruments may be inserted through the hysteroscope to help
treat any intrauterine pathology -
operative hysteroscopy . The recovery time is very quick. There is no
abdominal wound so there are no stitches and the postoperative pain is minimal.
Sexual intercourse is not advised for two weeks following the procedure. It is
advisable not to insert anything (besides the prescribed medication) into the
vagina for at least 2 weeks, including tampons.
Most women can return to work within 2 – 3 days.
|
 |
|
|
|